What was this study about?
Axial spondyloarthritis is a joint disease that affects the spine. It causes pain and disability, and is also associated with a number of other conditions – the eyes, skin and bowel are commonly affected. In the early 2000s new medicines became available, called ‘biologics’. These medicines have changed the way patients are managed, and there are now more than ten different biologic medicines available.
Data from clinical trials show that these medicines are effective. And indeed, positive results from several trials are required before a new medicine is licenced. However, clinical trials typically involve patients from only a small number of hospitals and, often, certain of patients are excluded – e.g. those with other conditions, and/or those who have previously received other similar medications. The clinical trial patients therefore don’t fully represent the entire patient population.
The purpose of the current study was to determine whether biologic medicines work as effectively as we expect ‘in the real world’, compared to data from clinical trials.
What did we do?
First, we wanted to determine how many patients starting biologic medicines would have been eligible for the clinical trials that were instrumental in the licensing of these medicines.
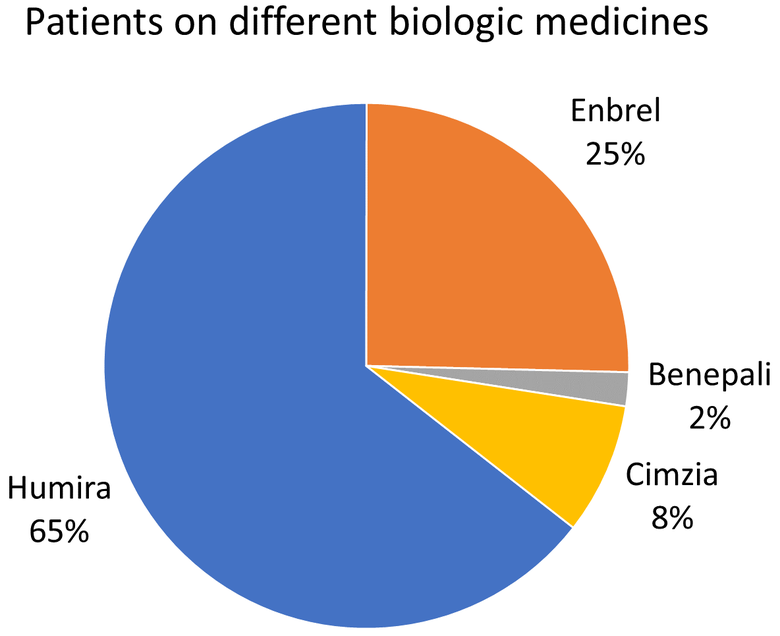
Using data from 83 hospitals across Great Britain (from the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis) we identified 816 patients who were starting biologic therapy. We then found all the relevant published clinical trials and looked to see which patients would / would not have been included.
Secondly, we wanted to see how many patients responded well to the biologics, compared to patients in the clinical trials.
What did we find?
We identified 14 relevant clinical trials. Where patients had been excluded, this was largely due to other medicines the patients were taking (or had taken), or a history of other health conditions. Of the 816 BSRBR-AS patients, nearly 60% would have been excluded from all of the relevant clinical trials.
In the clinical trials, nearly two-thirds of patients responded well to their biologic therapy. Whereas, in the BSRBR-AS , only half of patients reported an improvement in symptoms after one year.
What does this mean?
Doctors and patients should be aware that the chances of treatment success may be lower than the original clinical trials suggest. Future research should investigate why this is. By excluding patients with various other pre-existing health conditions, it may be that clinical trials give an over-optimistic estimate of the proportion of patients who will respond to treatment.
Who funded this work?
This study was supported by the British Society for Rheumatology who received funding for this from Pfizer, AbbVie and UCB.
Where can I read more?
To view the scientific paper, click here.
