
Lecturer
- About
-
- Email Address
- tara.sutherland@abdn.ac.uk
- Office Address
- School/Department
- School of Medicine, Medical Sciences and Nutrition
Biography
I graduated with a BSc with Honours degree from the University of Melbourne in Australia before embarking on PhD in Pharmacology studying oestrogen metabolites in cancer using breast tumour models. After a stint studying ligand-receptor modelling at Monash University, I moved to Edinburgh to begin learning all about immunology and how the lung responds to infections, allergens and injury.
I obtained an Asthma UK and Medical Research Fellowship and moved to the University of Manchester to develop and utilise models of allergic airway pathology to study immune responses and extracellular matrix remodelling in the lung. In 2022, I joined the University of Aberdeen, have a fantastic and growing research group who work on a central lab theme of uncovering key immuno-matrix networks that contribute to keeping our lungs healthy or drive development of disease.
NEW RESEARCH FINDINGS out in Science Immunology
Using models of severe allergic airway disease, we show that allergen-induced ECM remodelling occurs independently of IL-13 or IL-17 driven inflammation. Rather chitinase-like proteins drive airway ECM accumulation and inhibition of murine CLP Ym1 can remarkably reverse it
Latest Publications
Generation of a Ym1 Deficient Mouse utilising CRISPR-Cas9 in CB6 Embryos
Transgenic Research, vol. 34, 44Contributions to Journals: ArticlesAllergen-induced airway matrix remodeling in mice can be prevented or reversed by targeting chitinase-like proteins
Science Immunology, vol. 10, no. 111Contributions to Journals: Articles- [ONLINE] DOI: https://doi.org/10.1126/sciimmunol.adk6707
- [OPEN ACCESS] http://aura.abdn.ac.uk/bitstreams/218ba490-9880-4e45-978b-71f3a43cd3a3/download
- [ONLINE] View publication in Scopus
Generation of a Ym1 Deficient Mouse utilising CRISPR-Cas9 in CB6 Embryos
Working Papers: Preprint Papers- [ONLINE] DOI: https://doi.org/10.1101/2025.03.10.642405
An optimised faecal microRNA sequencing pipeline reveals fibrosis in Trichuris muris infection
Nature Communications, vol. 16, 1589Contributions to Journals: ArticlesExtracellular matrix phenotyping by imaging mass cytometry defines distinct cellular matrix environments associated with allergic airway inflammation
Working Papers: Preprint Papers- [ONLINE] DOI: https://doi.org/10.1101/2024.11.15.623782
- Research
-
Research Overview
The extracellular matrix (ECM) is the non-cellular part in all tissues and organs and is made up of molecules like glycosaminoglycans & proteoglycans (e.g. hyaluronan, chondroitin sulphate, heparin sulphate), fibrous proteins (e.g. collagen, elastin) and mucins. More than just physical architectural scaffold within our tissues, the matrix is biologically active with many functions including the ability to direct cell migration and influence cell function. In turn, tissues and immune cells provide critical cues that work together to maintain a healthy tissue matrix. However, if communication and interactions between the matrix and cells is compromised in light of infections, injury, inflammation or insults, tissue pathology ensues.
The Sutherland lab studies specifically focus on the lung, working at the interface between immunology and extracellular matrix biology. Our vision is to improve respiratory health by identifying the interactions between the physical tissue environment (e.g. ECM) and our immune system and why these interactions go wrong during disease.



The lab has diverse experience, inclusive and supportive environment that allows for imaginative research. I’m a big believer in providing a variety of career development opportunities and helping people succeed in their own goals.
Research Areas
Accepting PhDs
I am currently accepting PhDs in Biomedical Sciences.
Please get in touch if you would like to discuss your research ideas further.
Research Specialisms
- Allergy
- Biological Sciences
- Biomedical Sciences
- Immunology
- Pathology
Our research specialisms are based on the Higher Education Classification of Subjects (HECoS) which is HESA open data, published under the Creative Commons Attribution 4.0 International licence.
Current Research
Our team includes senior post-doc Matthew Burgess, PhD students Morgan Bryant and Andrew Love, and is held together with excellent technical help from Megan Robertson. Projects are supported by generous funding from Medical Research Scotland, University of Aberdeen Development Trust, Medical Research Council and Wellcome Trust. We use a range of cutting-edge technologies, bioinformatic analysis and immunological, biochemical assays that enable us to explore the lung tissue environment in various projects outlined below.
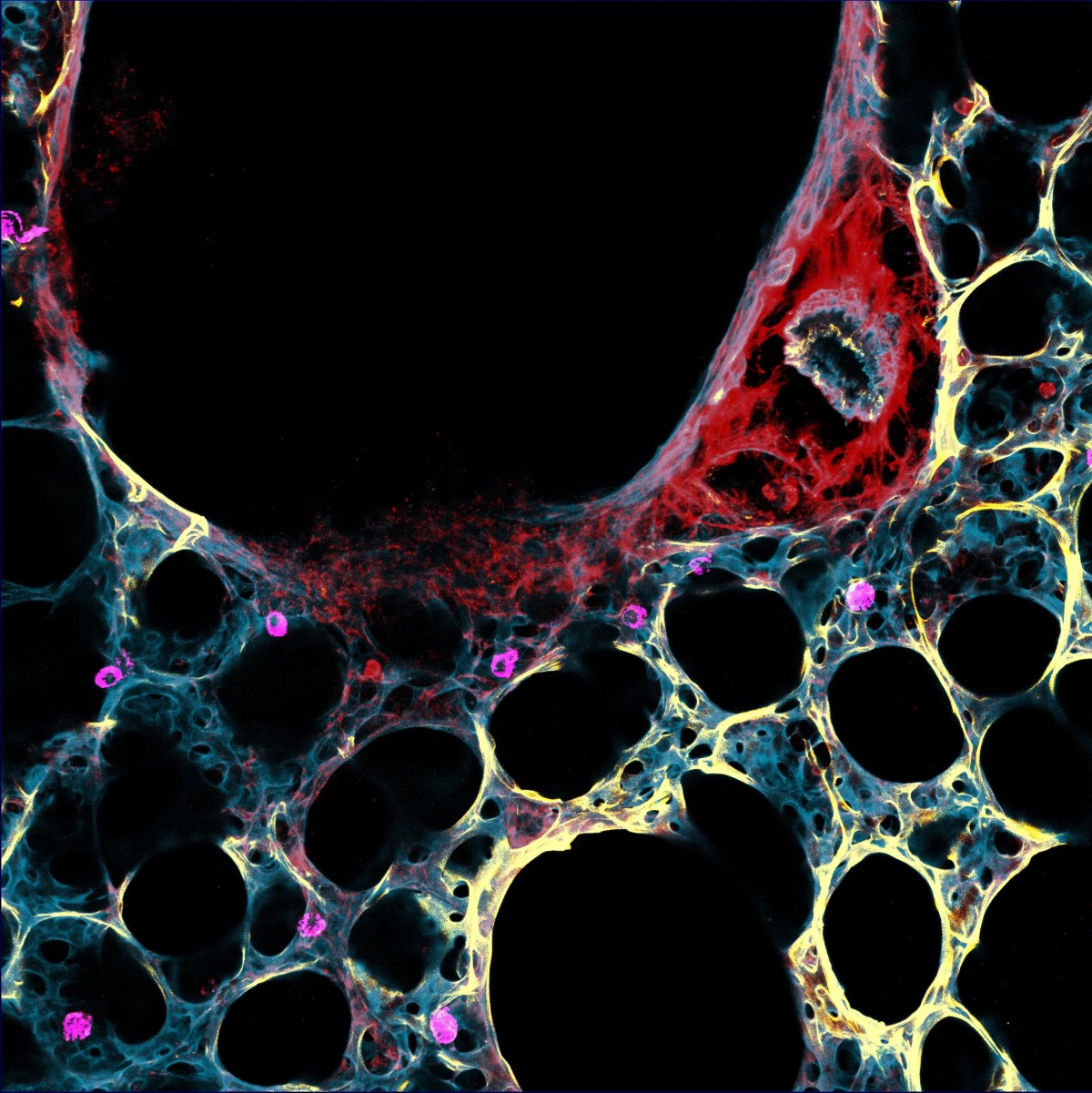
IL-13-hyaluronan axis during lung infection, injury, repair and fibrosis
The type 2 arm of the immune response is associated with both helminth infections and allergic inflammation but also critical in orchestrating tissue repair and fibrosis. However, we recently found that type 2 cytokine IL-13 as a driver of severe COVID-19 pathology through regulation of ECM component hyaluronan. Now we have funding from long-term funding Wellcome to mechanistically understand the IL-13-hyaluronan axis in the lungs, and why this pathway is important in pulmonary diseases. We are looking for a post-doc to join the team and work closely with collaborators at University of Manchester (Judi Allen, Tony Day and Tracy Hussell) and University of Virginia (William Petri). Lots of exciting potential to use spatial transcriptomics, high-dimensional imaging, and 3D cultures. Get in touch to discuss more - tara.sutherland@abdn.ac.uk.
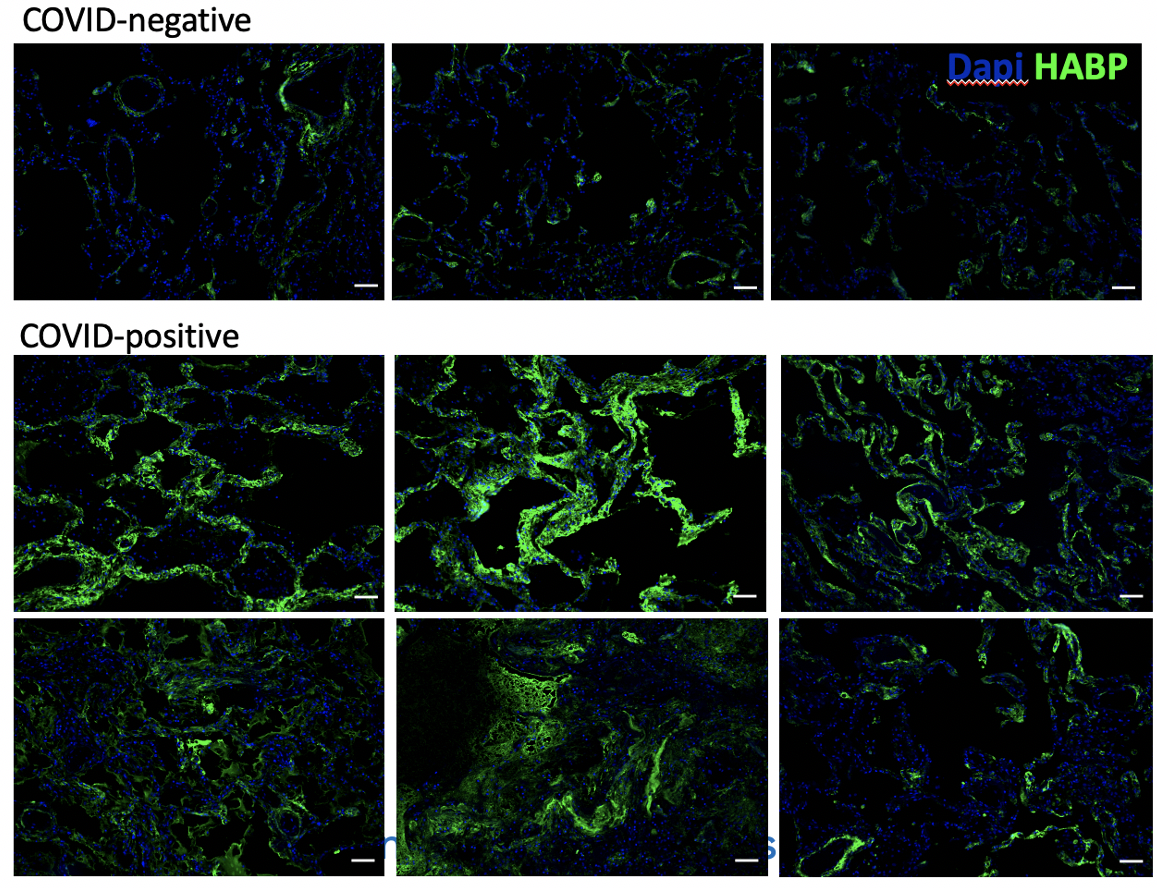
Immunostaining for hyaluronan (green) in the lungs from patients with or without
COVID-19. Donlan et al (2021) JCI Insights.Pathological matrix remodelling asthma: role for chitinase-like proteins, macrophages and fibroblasts.
Chitinase-like proteins (CLPs) are highly expressed during inflammation, tissue injury/repair and fibrosis. During helminth parasite infection, CLPs regulate immune responses and drive tissue repair. However, in more chronic settings like allergic airway pathology akin to asthma in people, CLPs are responsible for ECM remodelling in the lung, independent of effects on the adaptive immune response. Using animal models, human lung tissue resection, 3D lung slice cultures and a range of sophisticated techniques (e.g. microscopy, flow cytometry, scRNAseq, qPCR) we are exploring how CLPs influence the matrix, with a focus on macrophage-fibroblast cross-regulation. See our preprint that describes the ability of CLPs to influence ECM remodelling
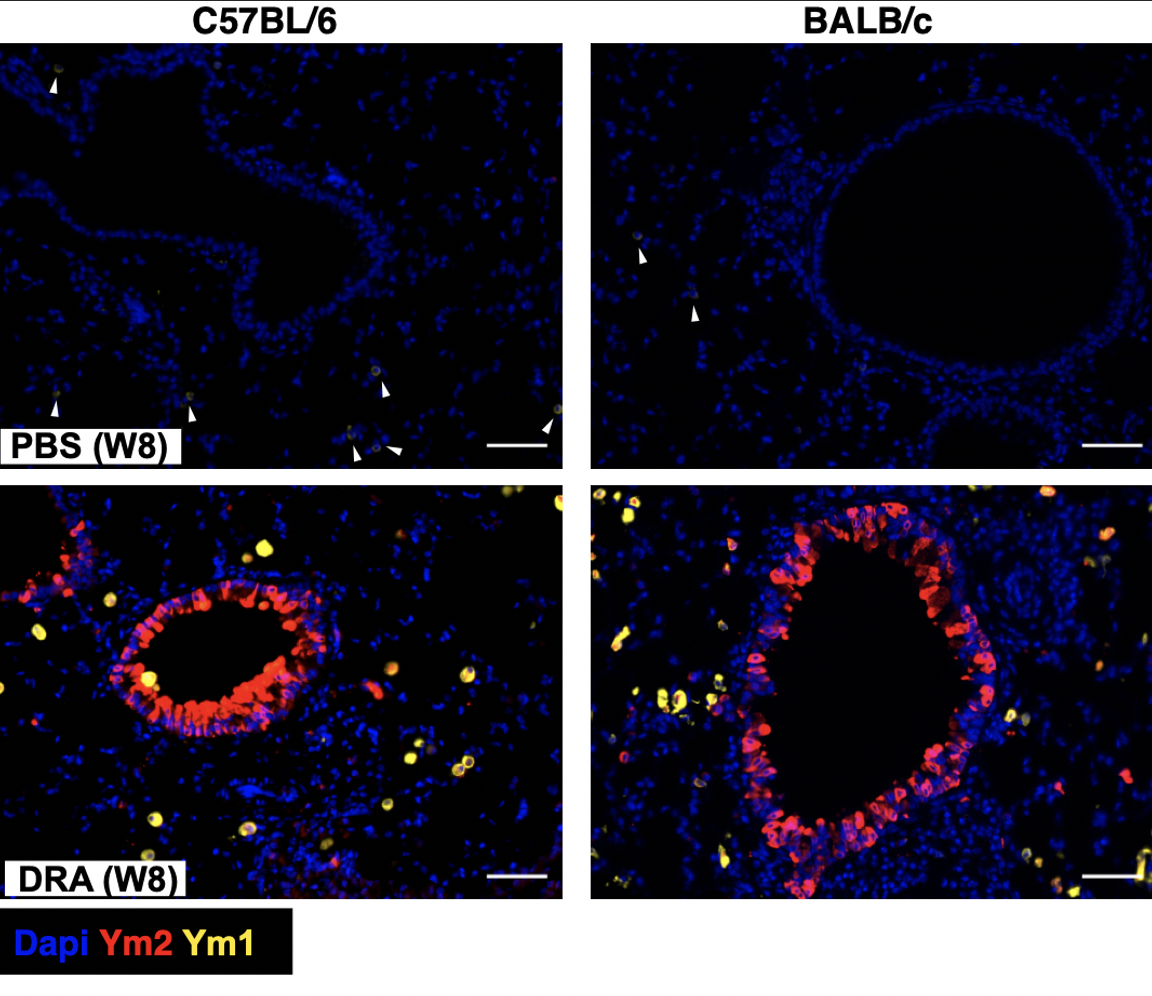
Increased expression of murine CLPs Ym1 and Ym2
following chronic administration of a cocktail of allergens
(DRA). Parkinson et al (2021) Immune Cell Biol.Characterising fibroblast dynamics during immune responses and lung pathology.
Fibroblasts are the most abundant cells within the tissue stroma, probably best known for their roles in synthesising and regulating the ECM. However, fibroblasts can also influence immune responses directly or indirectly. Conversely immune cells influence fibroblast function. We are using 3D lung slice cultures, advanced imaging and more traditional methods to investigate the different types of fibroblast populations found in the lung and whether the communication between fibroblasts and macrophages are influence by specific ECM environments.

Role of vascular remodelling in immune responses during allergic airway pathology
The airway vasculature serves many vital functions in maintaining lung health. However, during disease remodelling of the cells and matrix within and surrounding the vasculature will likely contribute inappropriate immune responses, and remodelling and hyper-reactivity of the airway during broncho-constriction. We are interested in understanding how pathogenic vascular remodelling changes the ability of the host to mount an appropriate immune response when faced with numerous challenges.
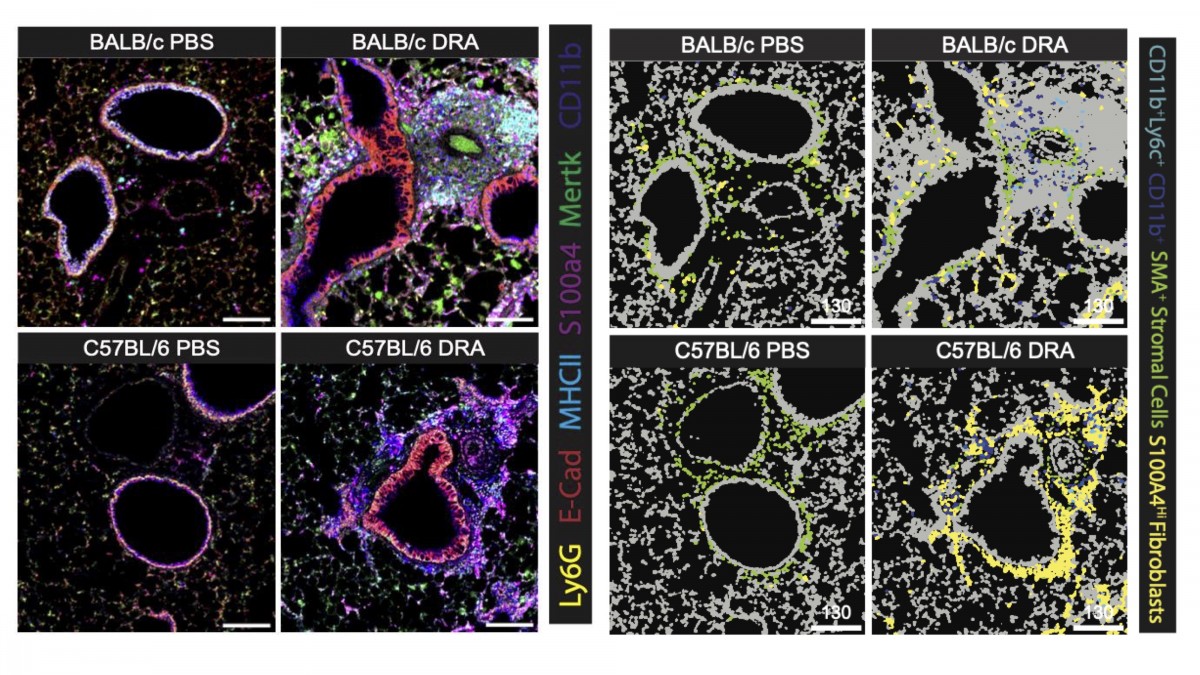
New analysis approaches to study ECM-cell interactions spatially in the tissue
New preprint shows cellular and ECM organisation in the lung during allergic pathology using imaging mass cytometry. We used methods to integrate analysis of cell segmentation and spatial ECM composition to ask questions about the lung environment during health versus pathology and how cell-cell and cell-ECM organisation changes.
Supervision
My current supervision areas are: Biomedical Sciences.
Current PhD students in the lab
James Parkinson - University of Manchester (part-time started in 2022)
Morgan Bryant - University of Aberdeen (started in 2023)
Andrew Love - University of Aberdeen (started in 2024)
Constantin Doerner - University of Aberdeen with Karolin Hijazi's lab (started in 2024)Recently graduated
Dr Hannah Tompkins - Wellcome Trust Immuno-matrix in complex disease; University of Manchester
Hannah recently passed her viva without corrections and was the first graduate of the Sutherland Lab!Funding and Grants
Medical Research Scotland (Jan 2024- July 2025) - Using human and mouse 3D lung tissue cultures to study immune cells and extracellular matrix organisation
Medical Research Council (April 2024 - April 2027) - Cell-matrix cross-talk in lung pathology and the role of chitinase-like proteins
Wellcome Discovery Award (Feb 2025 - Feb 2031) - Immune regulation of the hyaluronan matrix during lung infection, injury and repair - Publications
-
Page 1 of 5 Results 1 to 10 of 46
Generation of a Ym1 Deficient Mouse utilising CRISPR-Cas9 in CB6 Embryos
Transgenic Research, vol. 34, 44Contributions to Journals: ArticlesAllergen-induced airway matrix remodeling in mice can be prevented or reversed by targeting chitinase-like proteins
Science Immunology, vol. 10, no. 111Contributions to Journals: Articles- [ONLINE] DOI: https://doi.org/10.1126/sciimmunol.adk6707
- [OPEN ACCESS] http://aura.abdn.ac.uk/bitstreams/218ba490-9880-4e45-978b-71f3a43cd3a3/download
- [ONLINE] View publication in Scopus
Generation of a Ym1 Deficient Mouse utilising CRISPR-Cas9 in CB6 Embryos
Working Papers: Preprint Papers- [ONLINE] DOI: https://doi.org/10.1101/2025.03.10.642405
An optimised faecal microRNA sequencing pipeline reveals fibrosis in Trichuris muris infection
Nature Communications, vol. 16, 1589Contributions to Journals: ArticlesExtracellular matrix phenotyping by imaging mass cytometry defines distinct cellular matrix environments associated with allergic airway inflammation
Working Papers: Preprint Papers- [ONLINE] DOI: https://doi.org/10.1101/2024.11.15.623782
Injury From Nematode Lung Migration Induces an IL-13-Dependent Hyaluronan Matrix
Proteoglycan Research, vol. 2, no. 4, e70012Contributions to Journals: ArticlesIL-13 MODULATES THE HYALURONAN MATRIX FOLLOWING INJURY BY THE LUNG MIGRATING NEMATODE NIPPOSTRONGYLUS BRASILIENSIS
Proteoglycan ResearchContributions to Journals: ArticlesThe IL-17A-neutrophil axis promotes epithelial cell IL-33 production during nematode lung migration
Mucosal Immunology, vol. 16, no. 6, pp. 767-775Contributions to Journals: ArticlesAllergen-induced airway matrix remodelling in mice can be prevented or reversed by targeting chitinase-like proteins
Working Papers: Preprint Papers- [ONLINE] DOI: https://doi.org/10.1101/2023.08.18.553857
The extracellular matrix and the immune system: A mutually dependent relationship
Science, vol. 379, no. 6633, eabp8964Contributions to Journals: Review articles
