Optimizing intervention strategies via social prescribing as a means of encouraging and enabling healthy and sustainable dietary behaviours in individuals from low-income families.
This RESAS-funded 5 year project aims to support individuals from low-income families to change their food and eating practices in ways that are beneficial to health.
About the project
- Project summary
-
Our research
Adults and children living on a low income are more likely to be overweight or obese in Scotland than those living in less deprived circumstances. It has been estimated by the UK Food Foundation that the poorest fifth of Britain's population would have to spend 47% of their household income (after housing costs) to purchase food that meets Government recommendations for a healthy diet, and in light of this, the costs associated with consuming a healthy diet have been linked to weight gain in poorer households. In the past two decades a range of different programmes and approaches have been introduced to encourage and enable poor households to improve dietary intakes with limited success.
Our 5-year research programme is a collaboration involving the Rowett Institute, the University of Aberdeen, Robert Gordon University and Aberdeen City Council Health and Social Care Partnership. The overall aim is to explore the potential of social prescribing in connecting low-income clients with an expanded range of supports including community food programmes to help improve the range and quality of food consumed at home. Our research focus is located within Aberdeen City where social prescribing has been implemented with the support of the link practitioner programme for the last 5 years. This Scottish Government funded research has been undertaken to inform policy and practice associated with weight management programmes targeting deprived populations, and to address dietary inequalities in low-income groups more generally.

Project outline
The project has two main aims:
- Find out what community initiatives are currently running in Aberdeen city that are intended to support positive changes to food practices for low-income households and map out the content of these initiatives.
- Take the best parts from these existing initiatives and combine them with elements that we know (a) are helpful when we want people to change their behaviour and (b) the community wants. We will use all of this to create a tool for social prescribers that can be used to support people to make positive changes to their diet.
- What is social prescribing?
-
Social prescribing is a means for health professionals to refer people to a range of local, non-clinical services to improve health and well-being. The referrals generally, but not exclusively, come from professionals working in primary care settings, such as GPs or practice nurses.
Social prescribing recognises that people's health and well-being are determined mostly by a range of social, economic and environmental factors and aims to address people's needs in a holistic way. It also aims to empower individuals to take greater control of their own health.
There are various social prescribing models, with different referral routes. Many involve people being referred to a link practitioner, who considers their needs and then “prescribes” or links them to appropriate local support services or resources, typically provided by voluntary and community sector organisations. A “social prescription” can be, for example, a referral to a walking group, an emotional support group, a befriending service, housing advice, a cookery class, gardening or art activities.
Social prescribing schemes have primarily focused on improving mental and physical health, generally targeting people from lower-income communities who have a higher risk of suboptimal nutrition. Therefore, social prescribing could provide a promising platform to support improved eating practices in their client households.
- Events
-
Aberdeen Mela One World Day - 27 August 2023
We presented our SPICE Project at Aberdeen Mela- One World Day on Sunday 27 August 2023, during which we shared our Map of food-related services available in Aberdeen with the public and discussed people's experiences, views and needs regarding local food-related community services.
The team is very grateful for the high engagement and valuable input received from the public, with over 150 people contributing to our activities and asking questions about our project.

37th Annual Conference of the European Health Psychology Society - September 2023
Dr Julia Allan, Dr Oana Petre and PhD student Abigail Stephen from the SPICE group attended the Annual Conference of the European Health Psychology Society from 4-8 September 2023 in Bremen to present some of the preliminary findings from our studies in the project.

Voluntary Health Scotland (VHS) Annual Conference - 25 October 2023
Dr Oana Petre attended the Voluntary Health Scotland (VHS) Annual Conference - 'The Health Creators Summit' held in Edinburgh on 25 October. Our SPICE project was among the sixth finalists for the Annual Poster Competition. Oana has written a blog about her experience of attending the conference.

Social Inclusion and Cultural Diversity Research Impact Showcase event - 8 March 2024
Dr Frank Thies and Dr Oana Petre presented our SPICE Project at the University's International Women's Day celebrations, the Social Inclusion and Cultural Diversity 'Research Impact Showcase event on 8 March 2024.

UK Society for Behavioural Medicine Conference - 13 March 2024
Dr Oana Petre and PhD student Abigail Stephen travelled to Glasgow to present some of our research for the annual UKSBM conference on 13 March 2024.

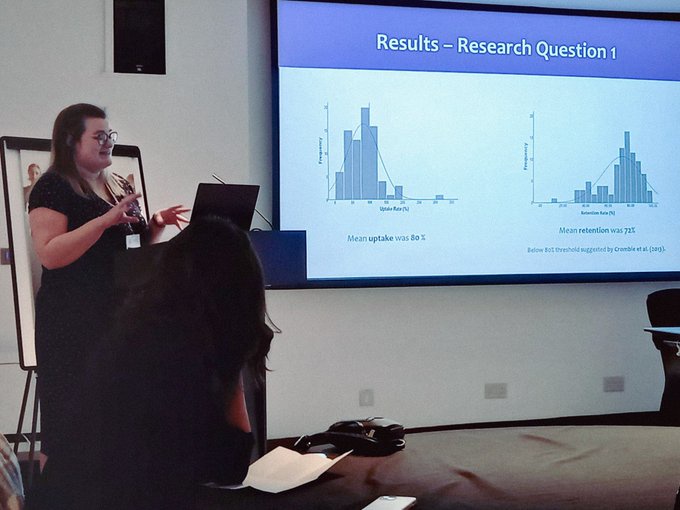
Scottish Public Health Conference - 1 May 2024
Dr Oana Petre attended the Scottish Public Health Conference on 1 May 2024 and presented some of our key findings from the interview study conducted with link practitioners.
Social Prescribing Meeting: Sharing Practices and Fostering Collaboration - 9 May 2024
On the 9th of May, we organised a meeting with social prescribing programme representatives and researchers from across Scotland to share insights into their practices, experiences, and challenges. By fostering collaboration and knowledge exchange, the event aimed to explore strategies for overcoming barriers and maximising the impact and sustainability of social prescribing in promoting health and wellbeing within our communities.
There was a clear consensus that we need a framework to ensure that all programmes follow similar guidelines for effective evaluation.
The team is very grateful to all participants for their invaluable insights.

- Contact us
-
Frank Thies
- Email: f.thies@abdn.ac.uk
- Telephone: +44(0)1224 437954
Oana Petre
- Email: oana.petre@abdn.ac.uk
- Telephone: +44(0)1224 438581
Address
The Rowett Institute, Foresterhill, Aberdeen AB25 2ZD University of Aberdeen
X / Twitter
Vist our X / Twitter profile: @SPICE Aberdeen
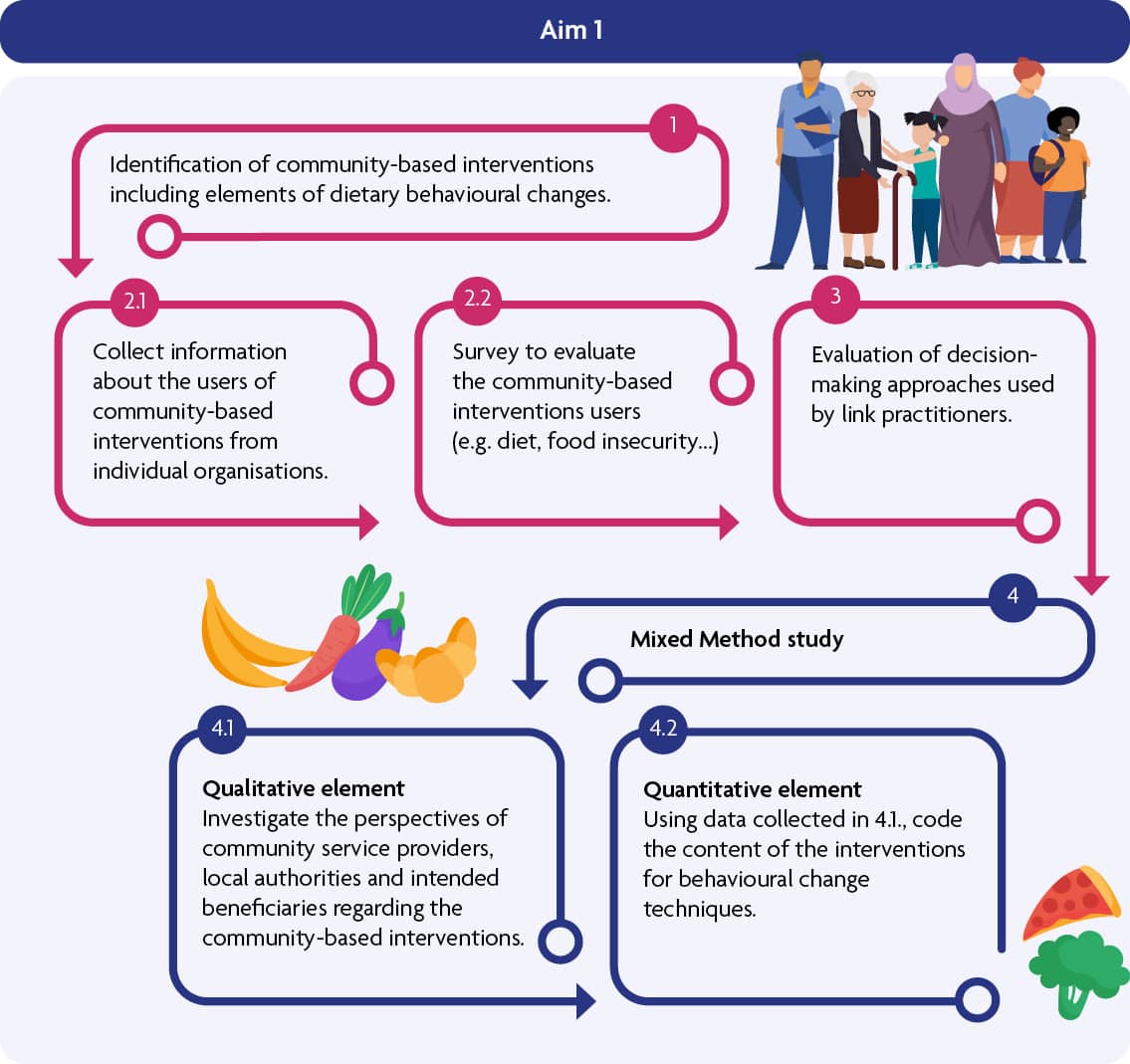
Aim 1
Find out what community initiatives are currently running in Aberdeen city that are intended to support positive changes to food practices for low-income households and map out the content of these initiatives.
- Objective 1
-
In collaboration with stakeholders involved in the Aberdeen City Health and Social Care Partnership, we mapped the full range of food access, with a particular interest in food-related community initiatives delivered in Aberdeen.
- Objective 2.1
-
We retrieved and analysed relevant information about clients from the community initiatives identified in Objective 1 to better understand the clients' characteristics and identify what things could be put in place to help them improve their eating habits.
Please contact one of the study leads for further information.
- Objective 2.2
-
The present study aimed to assess and characterise the individuals currently using community initiatives that focus on healthy food or dietary behavioural change and are available for the link practitioners from Aberdeen City to refer potential clients to them. The findings will give us a better understanding of the potential client group and inform the development of a social prescribing toolkit.
Between October 2022 and June 2023, we conducted a cross-sectional survey using a convenience sampling method (N=105). Participants were recruited through community initiatives providers. The questionnaire evaluated users' level of food insecurity experience, diet quality, mental health, well-being, intention and self-efficacity toward healthy eating and socio-demographic characteristics.
Results coming soon.
- Objective 3
-
Social Prescribing connects primary care patients with non-medical sources of support within the community. There are various SP models, with different referral routes. Many involve patients being referred to a link practitioner, who considers their needs and then “prescribes” or links them to appropriate local support services or resources, typically provided by the third sector.
The present study aimed to explore the Social Prescribing process and the decision-making of link practitioners, particularly around food and physical activity practices.
Sixteen semi-structured interviews were conducted with link practitioners working across Aberdeen City. A constructivist grounded theory approach informed study design, data collection, and analysis.
The study provides insight into the practical reality of making social prescription decisions, and has potential to inform training and evaluation processes and support the development of SP interventions.
Results coming soon.
- Objective 4
-
The main aim of this study is to evaluate existing community-based and food focused interventions delivered in Aberdeen City in order to identify those that (a) contain effective behaviour change techniques, and (b) people from low-income families value and engage with.
Adopting a mixed methods approach, this study will have two stages. Initially (qualitative element), we aim to investigate the views and perspectives of multiple stakeholders (i.e., community service providers, local authority members, local community members and intended beneficiaries) regarding the content and delivery of existing community-based interventions, operating in Aberdeen city, that support low-income communities access to food and resources that enable or encourage healthier food practices. In the second part of the study (quantitative element), we aim to code the content of the interventions (based on the comprehensive descriptions collected in the qualitative element) for behaviour change techniques using the BCT taxonomy v1 in order to identify the likely mechanisms underpinning any successful change in recipient's behaviour.
- Objective 4.1
-
Qualitative element
The qualitative element of the study will be conducted using principles and techniques found in Grounded Theory and ethnographic approaches. We will investigate views and perspectives from multiple stakeholders (i.e., community service providers, local authority members, local community members and beneficiaries) regarding the food-related community-based interventions available.
Based on the findings of this element, we will be able to determine which interventions appear most promising in terms of their: 1. pre-existing components, 2. intervention logic and concomitant community and socio-economic contexts, 3. intervention reach, and beneficiary-determined assessment of 4. acceptability and 5. perceived usefulness.
- Objective 4.2
-
Quantitative element
The interventions currently delivered within this community are diverse, multi-component and delivered by a range of different organisations and individuals. Therefore, is essential to identify interventions' “active ingredients” - the likely mechanisms underpinning any successful change in behaviour regardless of contextual differences in delivery. Thus, in the second part of the study (1.2. quantitative element), based on the comprehensive descriptions collected in 4.1 (qualitative element), the content of the interventions will be coded for behaviour change techniques (BCTs) using the BCT taxonomy v1.
BCT(s)= the smallest components of behaviour change interventions that on their own in favourable circumstances can bring about change. The defining characteristics of a BCT are that it is: “observable, replicable, irreducible, a component of an intervention designed to change behaviour, and a postulated active ingredient within the intervention”(1 )
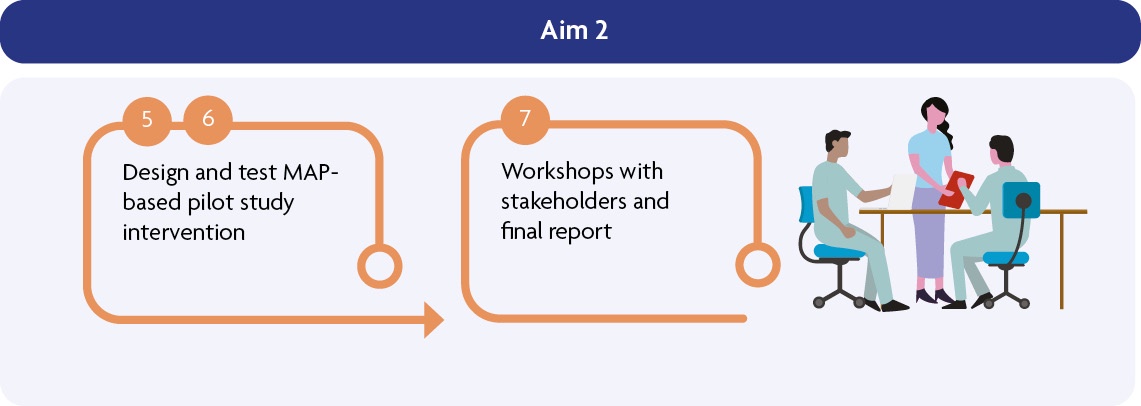
Aim 2
Take the best parts from these existing initiatives and combine them with elements that we know (a) are helpful when we want people to change their behaviour and (b) the community wants. We will use all of this to create a tool for social prescribers that can be used to support people to make positive changes to their diet.
- Objective 5
-
Using the information collated from the mixed method study (objective 4), and in consultation with Council Local Authority/Third Sector and NHS representatives, stakeholders and users, we will design a MAP-based optimised intervention. The optimised intervention will therefore build on the intervention components most likely to successfully change behaviour within this community (4.2; BCT coding work) and the components most likely to be valued and welcomed by members of the community (4.1; qualitative work).
The MAP (Motivation, Actions & Prompts) of Health Behaviour Change is the NHS Education for Scotland (NES) Learning Programme for all health and care practitioners whose role provides them the opportunity to help people make positive health and lifestyle related changes. The programme aims to give practitioners skills and confidence to notice, discuss and support opportunities for patients to make and maintain behaviour changes (2 ).
- Objective 6
-
We will carry out a MAP-based pilot intervention study, in collaboration with link practitioners and selected providers using the newly designed optimised approach and collect data on eating behaviour change, mental health and well-being status, weight, diet, physical activity, blood pressure and systemic biomarkers (HbA1C, carotenoids/tocopherols and vit D).
The MAP (Motivation, Actions & Prompts) of Health Behaviour Change is the NHS Education for Scotland (NES) Learning Programme for all health and care practitioners whose role provides them the opportunity to help people make positive health and lifestyle related changes. The programme aims to give practitioners skills and confidence to notice, discuss and support opportunities for patients to make and maintain behaviour changes (2 ).
- Objective 7
-
We will prepare the final report and organise a workshop with Council and NHS representatives, stakeholders and users, to present and discuss our findings and to evaluate potential impact on practices.
PhD project
This PhD project is running in parallel with the main RESAS-funded interdisciplinary research programme. It is complementary to the SPICE parent project and aims to provide more of an understanding of the client perspective.
The project's primary aim is to investigate factors associated with the uptake and engagement of community dietary interventions in lower income communities, specifically with those that can be recommended to clients via social prescribing initiatives. This will help to inform the development and design of an engaging social prescribing toolkit for link workers to use to support dietary behaviour change for low-income communities.
- Objective 1
-
To establish if existing community dietary interventions are successful in recruiting and sustainably engaging individuals from low-income communities, and if so what mode(s) of engagement and delivery are associated with successful uptake and engagement.
To achieve this objective, a systematic review is in progress; literature related to dietary interventions targeted at low-income groups has been collected and will be used to identify mode(s) of delivery associated with higher engagement. At this stage, a protocol has been registered with PROSPERO and data extraction is in progress.
- Objective 2
-
To understand the perspective of users and non-users of community dietary interventions within low-income communities, specifically what barriers and facilitators are associated with their uptake and engagement
To achieve this objective, we plan to conduct two studies. Firstly, a qualitative interview study will be used to understand barriers and facilitators experienced by the intended beneficiaries when accessing community dietary interventions. Secondly, a survey will be conducted to help understand factors associated with engagement and non-engagement with such interventions in users and eligible non-users. This survey will be based on the COM-B model.
- Objective 3
-
To identify the challenges faced by low-income communities when trying to secure food access during a cost-of-living crisis.
To achieve this objective, a photo-elicitation study will be conducted. Participants from low-income communities will be invited to share insight into their daily life by documenting how they secure food access during the ongoing cost-of-living crisis. Participants will photograph the food they access during a typical week, and then use these as prompts in a follow-up interview to explain the challenges they face and how they affect the foods they consume.
- Objective 4
-
Using intervention mapping, to formulate recommendations for components of a novel social prescription toolkit that is intended to improve diets in low-income communities
To achieve this objective, the findings from objectives 1-3 will be used to design a potential intervention. An intervention mapping approach will be implemented to inform the development of a novel social prescription toolkit. These recommendations will then be considered in the development of the SPICE social prescribing model for the parent RESAS project.







