It is estimated that as many as between 3 million and 6 million people in the UK experience some degree of urinary incontinence. There are several types of incontinence. Stress incontinence is one of the main trypes. It is caused by sphincter weakness and occurs when there is pressure on the abdomen created by sneezing, coughing, lifting, or straining. The second common type is urge incontinence, caused by bladder abnormalities leading to an irresistible urge to pass urine. The third main type is mixed incontinence which is a combination of stress and urge.

Treatments
Urinary incontinence impacts on people’s quality of life by affecting their physical and psychological well-being. It can lead to embarrassment, low self-esteem and social isolation. There are several treatments that are available depending on the severity of the urinary incontinence. Initially, the doctor may suggest some simple measures, for example, use of incontinence products such as pads, or lifestyles changes including losing weight and reducing intake of coffee and alcohol. Other conservative measures include pelvic floor muscle training where patients strengthen the pelvic floor muscles by squeezing them, or bladder training where patients learn to wait longer between needing to and passing urine. Patients may also use drugs to control their incontinence.
Surgical interventions are offered if the symptoms persist depending on the type of incontinence.
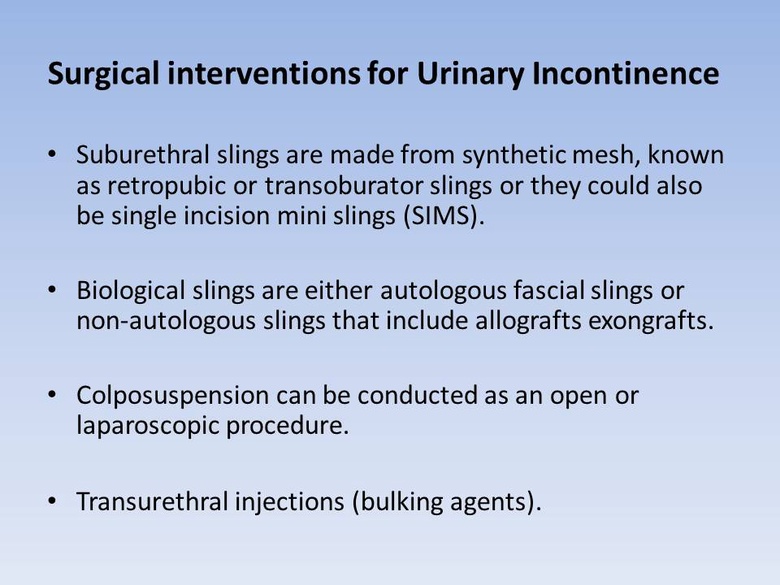
Stress incontinence surgical interventions aim to strengthen the muscles that control the flow of urine or reduce pressure on the bladder. Urge incontinence surgery aims to enlarge the bladder or to stimulate the nerve that controls the detrusor muscle. This muscles controls the storage and release of urine.
The high prevalence of urinary incontinence results in a high overall cost of treatment and containment. The surgical procedures are relatively invasive operations and are costly. This limits the number and type of patients that can be treated within the resources available.
Urinary Incontinence research at HERU
HERU has conducted studies that have explored the cost effectiveness of both surgical and non-surgical interventions of urinary incontinence. As urinary incontinence is a chronic and progressive disease there is a need to analyse not only the cost effectiveness of specific interventions but also to explore the cost effectiveness of different care pathways that patients experience when receiving treatment. This blog briefly describes two of our studies.
Non-surgical - OPAL
The first study looks at a non-surgical intervention. Pelvic floor muscle training (PFMT) exercises are taught by a specialist physiotherapist or nurse. There is evidence that these exercises can strengthen muscles and decrease leakage. Current UK guidelines recommend that the women are offered at least three months of pelvic floor muscle exercises. However, it is not clear how "intensively" women have to exercise to get a good result that lasts.
The Optimal PFMT for Adherence Long-term (OPAL) trial aimed to find out whether the use of biofeedback can help to improve the results of PFMT exercises in the short- and longer-term. Using a probe inserted into the vagina, biofeedback equipment shows women what their pelvic floor muscles do. Women were allocated at random to one of two groups, either the usual exercise programme recommended by the UK guidelines (called basic exercise) or the same exercises with the addition of biofeedback (called intensive exercise). Both groups of women were to visit a specialist nurse or physiotherapist six times in 16 weeks to be taught the exercises and encouraged to use them.
An economic evaluation was conducted alongside a randomised controlled trial that investigated whether biofeedback-mediated intensive PFMT was more effective and cost-effective than basic PFMT for the treatment of female stress or mixed urinary incontinence. The cost effectiveness analysis measured the costs and benefits of these treatments to determine the incremental cost per quality adjusted life year (QALY) gained at 24 months. The report is currently awaiting publication. Details can be found at the HTA Journals website.
Surgical - SIMS
The second study is also being conducted alongside a randomised controlled trial. The study investigates two surgical interventions, adjustable anchored Single-Incision Mini-Slings (SIMS) and Standard tension-free Mid-Urethral Slings (SMUS) in the management of female stress urinary incontinence.
Cost effectiveness (cost per QALY gained) will be reported over a three year follow up period. Research suggests that the EQ-5D questionnaire used to measure the quality of life may not fully capture the benefits from successfully treating incontinence. Therefore, a discrete choice experiment will be conducted to measure patient preferences for the treatments and their associated outcomes.
We hope our research will provide decision makers with information on the cost effectiveness of these two treatments. The results will be published at the trial page on the HTA Journals website.
There is more information on these projects at the HERU urinary incontinence research webpage.
Many thanks to Mary Kilonzo of HERU for her work in developing this blog post.

HERU is supported by the Chief Scientist Office (CSO) of the Scottish Government Health and Social Care Directorates (SGHSC). The views expressed here are those of the Unit and not necessarily those of the CSO.


